The promise of a learning health system
For over two decades, thought leaders have described the promise of a learning health system, an ecosystem in which data drawn from the routine delivery of care continuously feeds back into improved decision-making, efficiency, and ultimately, better outcomes for patients. The Institute of Medicine first articulated this vision in 2007, emphasizing the potential for every patient’s experience to contribute to collective knowledge, and for that knowledge in turn to shape future care1. Oncology, with its complexity, rapidly evolving evidence base, and profound patient impact, was seen as a prime candidate for this transformation.
The barriers to realizing the vision
Yet almost 20 years later the vision has proved stubbornly difficult to realize. The challenge and cost of structured data capture has proved a major barrier. For oncologists, therapists, nurses and allied health teams, structured data entry required enormous effort. Documentation systems that were designed to facilitate analysis often only added to the administrative burden, siphoning time away from direct patient care2. The data itself was fragmented and unstructured, spread across disparate silos such as electronic medical records, imaging archives and pathology systems. Even when captured, data rarely flowed back into clinical workflow to support clinical decision-making at the point of care. Clinical trials and registries produced valuable insights, but on timescales of years rather than days or weeks3. In practice, the idea of a continuously learning health system felt out of reach.
The need for data-driven care in oncology is acute. Cancer treatment requires the coordination of large multidisciplinary teams, and decisions are influenced by a multitude of variables: tumor type and stage, comorbidities, genomic profiles, toxicity risks, patient preferences and available modalities. No single physician, however experienced, can fully synthesize this complexity unaided. Yet the alternative, burdening clinicians with ever more clinical complexity, administrative documentation and manual quality checks, is untenable. Already, oncologists report spending more time entering data than caring for patients. The result is a workforce stretched to breaking point, with productivity bottlenecks compounding as patient volumes rise.
The turning point: AI innovation
What has changed is the technology available to us. Advances in artificial intelligence (AI) and natural language processing now allow for the capture and structuring of clinical data directly from the point of care. Conversations between doctors and patients, dictated notes, pathology and imaging reports, all can be transformed into structured data without requiring a human to laboriously type codes into a form4. The potential for AI in health care is profound. AI models can now map clinical events against guidelines, detect gaps in documentation and offer recommendations consistent with the latest evidence5,9. They can flag risks, suggest treatment pathways and provide real-time decision support9. Critically, these tools operate not as point solutions, but within cloud-native workflows that make integration possible across the fractured oncology ecosystem. Cloud-based infrastructure allows scalability, interoperability and security while also enabling continuous updates. As new evidence emerges or as models are refined through local practice, improvements can be deployed seamlessly across an entire network.
Integrating intelligence across oncology workflows
This is where the new generation of data-driven systems demonstrates its value. By automating documentation and embedding evidence-based support into workflows, AI reduces administrative load while simultaneously improving quality. At the same time, by structuring and aggregating practice data, it enables the creation of real-world evidence at scale. Treatment patterns, comparative effectiveness, toxicity trends, and health economics outcomes, all become visible as part of everyday practice.
At Lumonus, this is precisely the future we are working to bring into reality. Our mission is to transform oncology workflows with technology that not only reduces administrative burden but also enhances clinical decision-making and accelerates learning. We built the Lumonus AI platform on a secure and scalable cloud-native infrastructure. We designed an Oncology intelligence layerTM that has 3 key components.
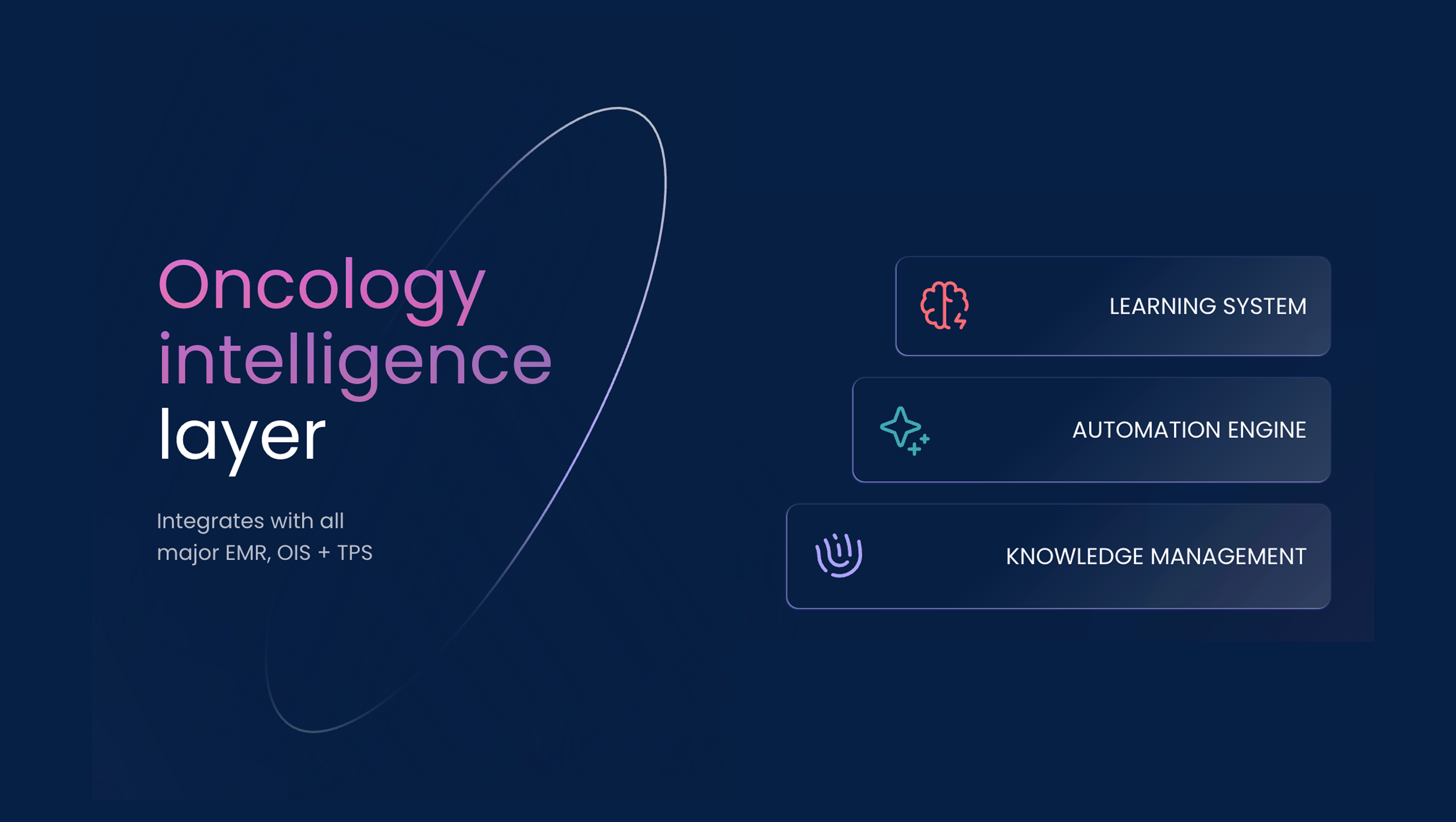
Oncology intelligence layer
- Knowledge management: Detailed clinical pathways and standard operating procedures to support quality and efficiency
- Automation engine: AI-powered workflows that automate routine tasks, reduce administrative burden and provide clinical decision support at the point of care
- Learning system: Embedded real-world data generation that arises naturally from the delivery of care. In this way, data collection ceases to be a burden; it becomes a byproduct of good clinical practice and can be leveraged to shape future patient care.
The Lumonus AI platform brings these ideas to life through key workflow stages consulting, prescribing, documentation, treatment planning and insights. Together, these tools reduce administrative friction, support evidence-based practice, and generate the structured data that underpins learning.
Efficiency, quality and continuous improvement
The benefits are tangible. Clinicians spend less time on repetitive tasks and more time with their patients. Treatment planning and documentation processes become faster and more reliable. Institutions gain immediate visibility into the quality and efficiency of their operations. And across the system, the capture of structured data enables the generation of real-world evidence on a scale that has long been imagined but rarely achieved. The vision of a true learning health system in oncology starts to move from aspiration to reality.
Economic and workforce impact
The case for adoption is compelling on multiple fronts. Economically, the oncology workforce is under pressure worldwide, with demand for clinical teams outpacing supply7. Automating repetitive and administrative elements of care alleviates these shortages while preserving quality. Value-based care models, increasingly emphasized by payers and regulators, depend on the collection of robust outcomes data, which our platform generates as a natural part of clinical workflows. Operationally, health systems face growing cost pressures, and the productivity gains offered by AI-powered workflows deliver relief without sacrificing safety.
Clinically, the benefits are just as clear. Standardization across sites ensures consistency of care regardless of geography or resources. Automated checks built into treatment planning reduce the likelihood of error and enhance safety8. And because the data is captured seamlessly from routine care, it reflects the diversity of real-world populations, not just the select cohorts included in clinical trials.
Policy alignment and global equity
Policy makers and regulators are also encouraging this direction. Agencies such as the FDA and EMA are increasingly recognizing the role of real-world evidence in regulatory approvals, coverage decisions, and safety monitoring6,10. Cloud-native, AI-powered platforms that can generate this evidence in a secure and compliant manner are therefore aligned with emerging policy priorities. At the same time, by democratizing access to decision support and best-practice workflows, these technologies can promote greater global equity in cancer care11.
Realizing the promise of data-driven cancer care
At Lumonus we believe that the historic vision of a learning health system is finally within reach. What was once constrained by the prohibitive cost of structured data collection can now be achieved with the aid of intelligent workflow, artificial intelligence and cloud-native infrastructure. At Lumonus, we are proud to stand at the forefront of this movement, embedding intelligence into oncology workflows so that data becomes a catalyst for better care. The time has come to move from aspiration to action - to realize the promise of data-driven cancer care for patients everywhere.
References
- Institute of Medicine. The Learning Healthcare System. Washington, DC: National Academies Press; 2007.
- Sinsky C, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165(11):753–760.
- Califf RM, et al. Transforming Evidence Generation to Support Health and Health Care Decisions. Sci Transl Med. 2012;4(125):125cm3.
- Rajkomar A, et al. Machine Learning in Medicine. N Engl J Med. 2019;380:1347–1358.
- Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25:44–56.
- Makady A, et al. Real-world data: RWD sources and regulatory use. Pharmacoepidemiol Drug Saf. 2017;26(12):1443–1453.
- Shah, Chirag et al The American Society for Radiation Oncology Workforce Taskforce Review of the United States Radiation Oncology Workforce Analysis. International Journal of Radiation Oncology, Biology, Physics, Volume 116, Issue 3, 484 - 490
- M.Price et al. 2023. Clinical Evaluation of an Automated Iterative Optimization System for Radiation Oncology. ASTRO 2023
- Mishra S, et al. AI in Oncology: Current Applications and Future Directions. Front Oncol. 2022;12:812785.
- Sherman RE, et al. Real-World Evidence — What Is It and What Can It Tell Us? N Engl J Med. 2016;375:2293–2297.
- Pramesh CS, et al. Equity in Cancer Care: Global Perspectives. Lancet Oncol. 2020;21(11):1459–1461.


